Introduction
svtsim is a web-based cardiac electrophysiology study (EPS)/arrhythmia simulator, which is primarily designed for training and education. In this article, we review how svtsim can be used to simulate common diagnostic maneuvers performed during an electrophysiology study. The interested reader is invited to supplement the discussion of each arrhythmia with running the simulator.
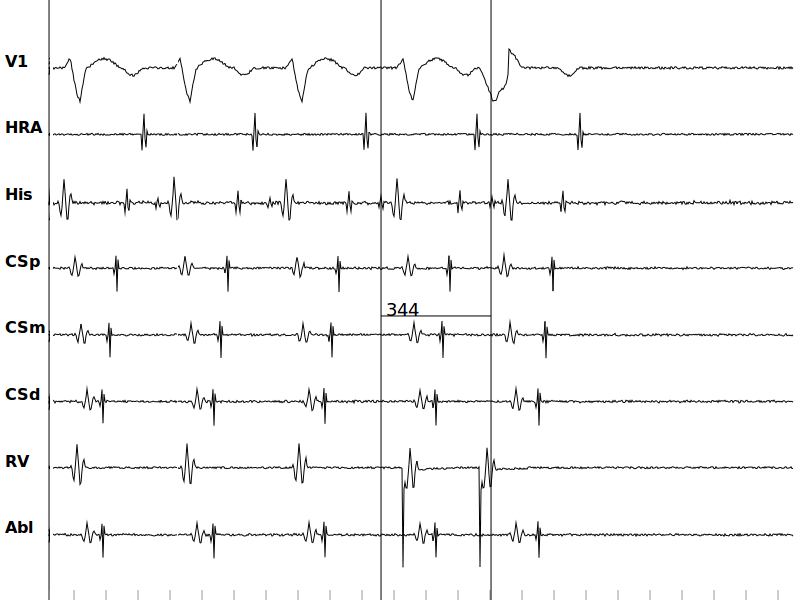
The starting point is normal sinus rhythm. In svtsim, various tachycardia models are built by modifying the sinus rhythm model. The top channel on the screen is a simulated surface ECG channel corresponding to lead V1. The intracardiac channels are located at high right atrium (HRA), His location (His), proximal/mid/distal coronary sinus (CSp, CSm, and CSd, respectively), and finally the right ventricular apex (RV). The Basic and Advanced screens are generally similar with the exception of an ablation channel (Abl) in some of the Advanced scenarios.
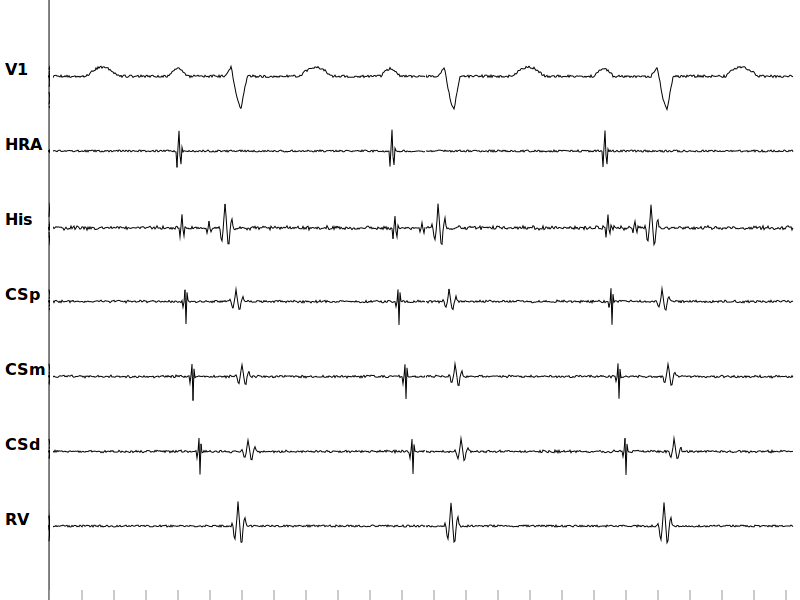
Simulated surface and intracardiac signals in the Normal sinus rhythm scenario.
Atrioventricular Nodal Reentrant Tachycardia (AVNRT)
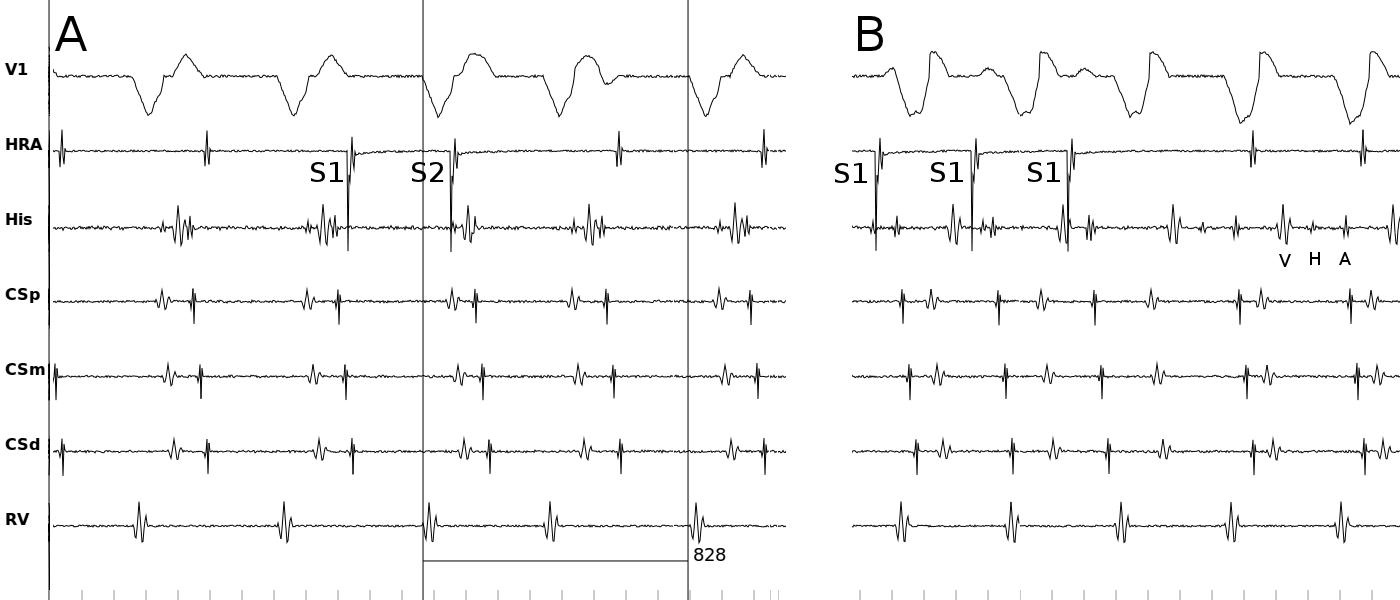
Addition of a slow pathway to the baseline (i.e. sinus rhythm) model creates the substrate for AVNRT. In the dual AV nodal physiology scenario, the refractory period of the slow pathway is set in a way to prevent sustained reentry. Delivery of extrastimuli with decremental coupling interval after a drive train demonstrates the presence of dual physiology with a jump in the AH interval.
- Select Dual AV Nodal scenario from the Advanced screen
- Set S1 ← 600 ms and S2 ← 400 ms
- Pace & Pause
- Decrease S2 by 10 ms and repeat until jump in AH is noted
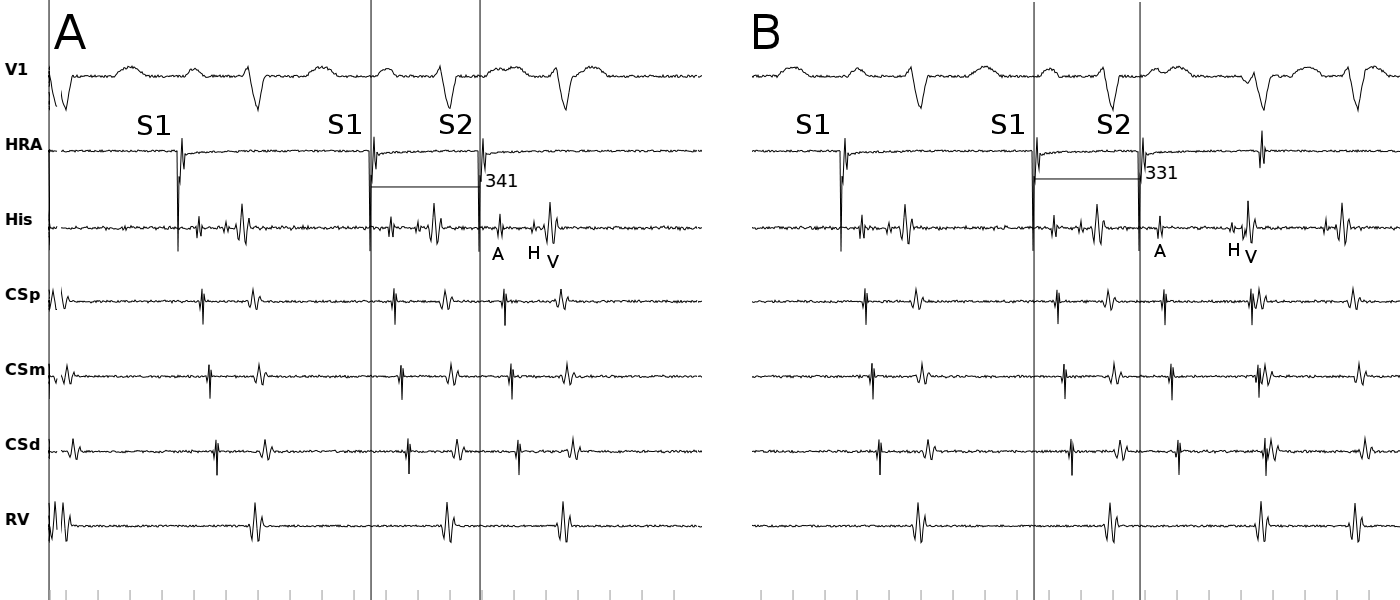
Simulated surface and intracardiac signals in the dual AV nodal pathway scenario. (A) Delivering a premature stimulus at coupling interval of 340 ms conducts down the fast pathway with a short AH interval. (B) A premature stimulus at coupling interval of 330 ms blocks in the fast pathway and conducts down the slow pathway with a long AH interval.
Modification of the slow pathway refractoriness makes reentry possible (AVNRT scenario). Now, a timely atrial extrastimulus blocks in the fast pathway and initiates reentry.
- Select AVNRT scenario from the Basic or Advanced screens
- Set S1 ← 600 ms and S2 ← 400 ms
- Pace & Pause
- Decrease S2 by 10 ms and repeat reentry is initiated
Ventricular overdrive pacing entrains the reentry with a VAV response, long post-pacing interval (PPI) and an increase in the VA timing (ΔVA>85 ms), all consistent with typical AVNRT (slow-fast).
- Select AVNRT scenario from the Basic or Advanced screens
- Induce tachycardia as above
- Pause and measure the tachycardia cycle length using the caliper
- Resume
- Set S1 10-20 ms shorter that the tachycardia cycle length
- Set the pace site at RV Apex
- Pace Straight until the tachycardia is entrained
- Stop Pacing and Pause immediately
- Confirm entrainment by measuring the A-A interval during pacing. It should be equal to the pacing cycle length
- Measure the post pacing interval from the last pacing stimulus to the first return signal on the RV channel
On the other hand, delivery of ventricular extrastimuli to the same model initiates atypical AVNRT (fast-slow) with prolonged VA interval. Ventricular overdrive pacing again entrains the reentry with a long PPI and a pseudo VAAV response. Note that the Induce Arrhythmia button in svtsim induces typical AVNRT in the Basic and atypical AVNRT in the Advanced screens.
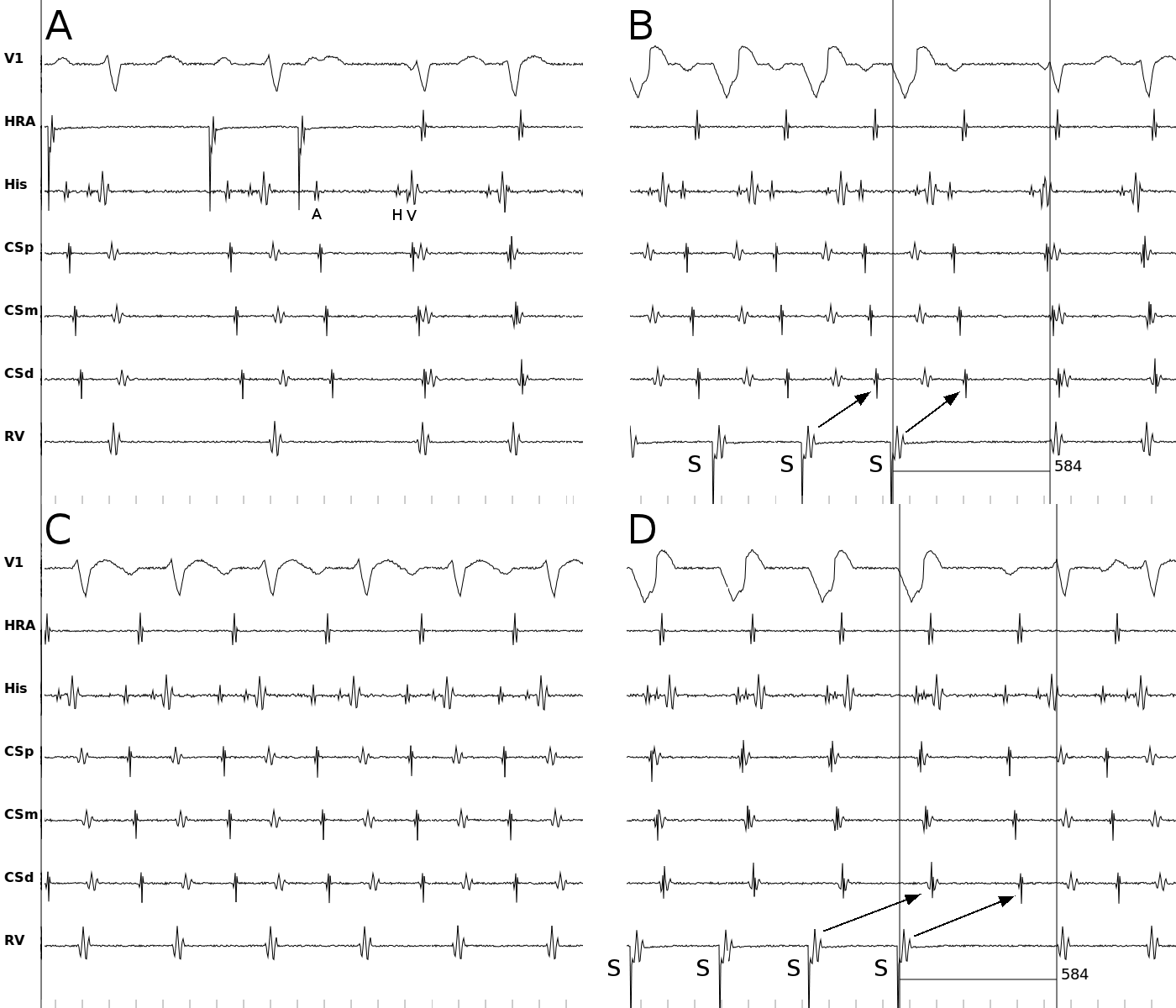
Simulated surface and intracardiac signals in the AVNRT scenario. (A) Delivering a premature stimulus at coupling interval of 330 ms blocks in the fast pathway, conducts down the slow pathway, and initiates typical AVNRT at a cycle length of 350 ms. Note the near simultaneous activation of atria and ventricles. (B) Ventricular overdrive pacing at a cycle length of 330 ms entrains the tachycardia. Note the VAV response, long PPI (134=584-350 ms), and ΔVA>85 ms, all consistent with typical AVNRT. (C) Atypical AVNRT in the same model. (D) Ventricular overdrive pacing entrains the tachycardia with a pseudo VAAV response due to long VA conduction. Arrows connects the ventricular paced beats to the corresponding atrial complexes.
Accessory Pathway Mediated Tachycardias
Accessory pathways are modeled as links between atria and ventricles. Addition of a non-decremental link between distal coronary sinus and adjacent ventricle creates the substrate for AVRT. Both unidirectional (concealed) and bidirectional (manifest) accessory pathways are implemented.
- Select AVRT scenario from the Basic screens or Concealed accessory pathway scenario from the Advanced screen
- Set S1 ← 600 ms and S2 ← 400 ms
- Pace & Pause
- Decrease S2 by 10 ms and repeat until tachycardia is initiated
Note the eccentric atrial activation pattern during tachycardia. Ventricular overdrive pacing entrains the tachycardia with relatively short PPI and (ΔVA<85 ms).
- Select AVRT scenario from the Basic screens or Concealed accessory pathway scenario from the Advanced screen
- Induce tachycardia as above
- Pause and measure the tachycardia cycle length using the caliper
- Resume
- Set S1 10-20 ms shorter that the tachycardia cycle length
- Set the pace site at RV Apex
- Pace Straight until the tachycardia is entrained
- Stop Pacing and Pause immediately
- Confirm entrainment by measuring the A-A interval during pacing. It should be equal to the pacing cycle length
- Measure the post pacing interval from the last pacing stimulus to the first return signal on the RV channel
The following figure shows an episode of orthodromic reciprocating tachycardia (ORT) using a concealed accessory pathway.
Simulated surface and intracardiac signals in the AVRT scenario. (A) ORT using a left lateral concealed accessory pathway with a cycle length of 345 ms. Note the eccentric atrial activation. (B) Ventricular overdrive pacing entrains the tachycardia with a VAV response and short PPI (83=428-345 ms).
A commonly used maneuver for differentiation of ORT from AVNRT is delivery of His-refractory PVC. A PVC that terminates the tachycardia or affects the subsequent atrial activity proves the existence of a retrogradely conducting accessory pathway. Note that the mere existence of an accessory pathway does not mean that it is involved in the tachycardia circuit. svtsim does not have an automatic feature for delivery of His-refractory PVC, but it is easy to emulated one as is described below.
- Select Concealed accessory pathway scenario from the Advanced screen
- Induce tachycardia as above
- Pause and measure VH interval (V in RV to H) using the caliper
- Resume
- Set S1 ← VH and the number of beats in the S1 train ← 2
- Set the pace site at RV Apex
- Set the sense site at RV apex
- Pace & Pause
- Measure HH to confirm His-refractoriness
- Measure AA interval
- Decrease S1 by 10 ms
- Repeat 8-11 until tachycardia terminates or AA changes
Simulated surface and intracardiac signals in the Concealed accessory pathway scenario. Delivery of a His refractory PVC terminates the tachycardia. Note that HH interval measurement (caliper) proves that the PVC was delivered while His was refractory. Termination of the tachycardia proves the existence of an accessory pathway; however, since the termination was after atrial activity, it does not prove that the accessory pathway is indeed involved in the reentry.
The simulator also exhibits "Coumel's Sign", where the prolongation of the VA interval (and usually the tachycardia cycle length) after spontaneous bundle branch block during ORT proves the existence and participation of an accessory pathway ipsilateral to the blocked bundle.
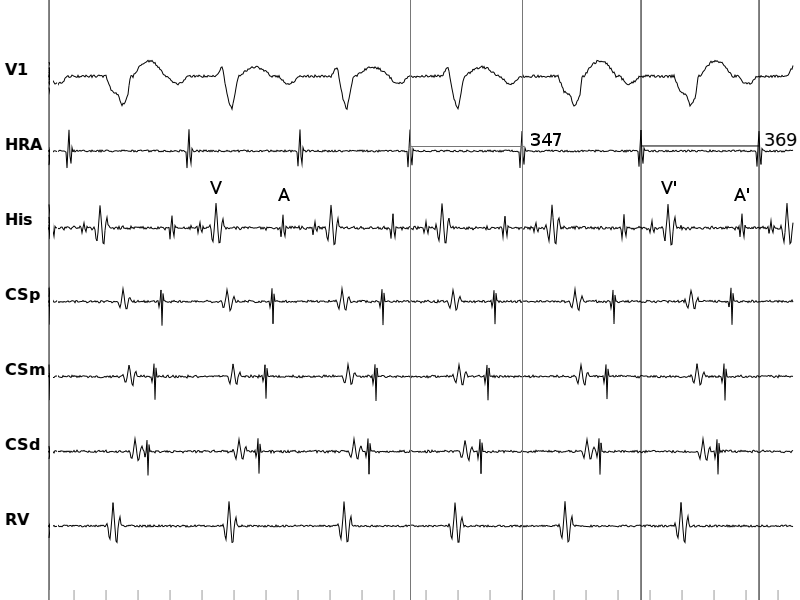
Simulated surface and intracardiac signals in the AVRT scenario with a concealed accessory pathway. Spontaneous LBBB occurs during tachycardia with the prolongation of the septal VA interval (V'A' compared to VA) and tachycardia cycle length.
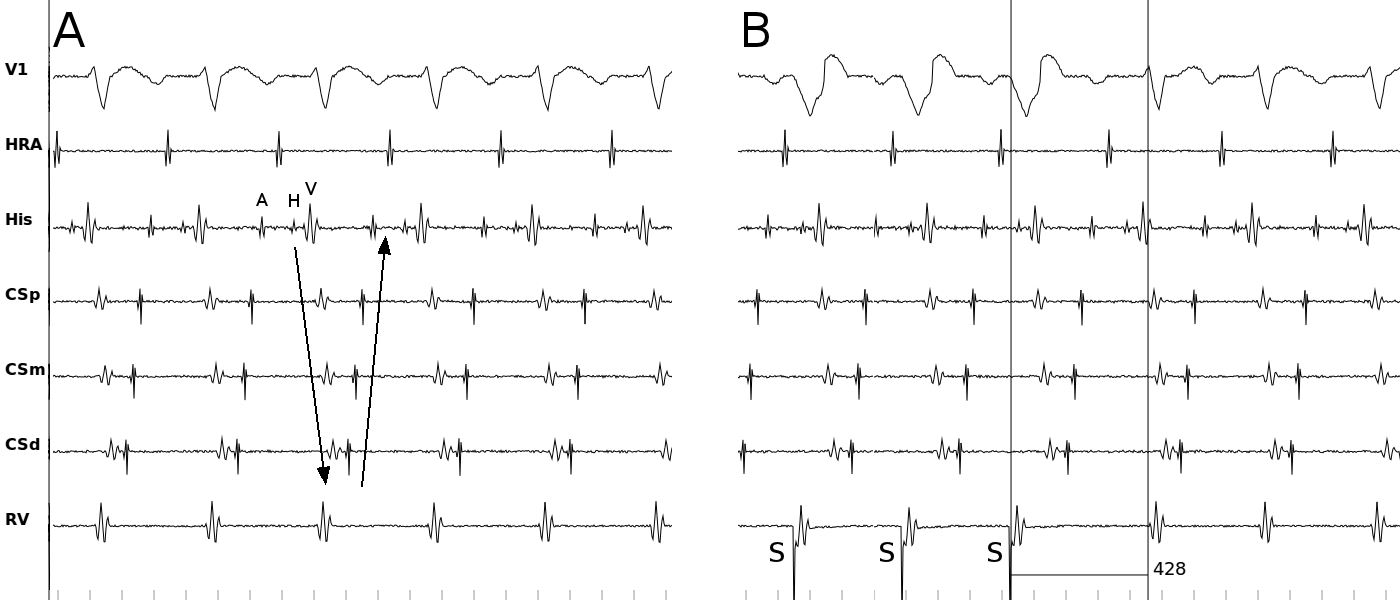
Septal pathways can be particularly difficult to diagnose. Multiple pacing maneuvers are developed to distinguish a septal pathway from AVNRT. In the presence of a non-decremental septal pathway, there is no significant different in the VA timing during either high-amplitude para-Hisian pacing (capturing both local ventricular tissue and the His bundle) and low-amplitude para-Hisian pacing (capturing only the local tissue). On the other hand, if the only connection between the ventricle and atria is through the AV node, high-amplitude pacing results in a shorter VA timing.
- Select Septal pathway scenario from the Advanced screen
- Select Pace location as "Para-Hisian (low output)"
- Set S1 ← 600 ms
- Pace straight
- Pause and measure VA interval in the His channel using the caliper
- Resume
- Stop pacing
- Select Pace location as "Para-Hisian (high output)"
- Repeat steps 3-7
- Compare VA timing during high-output pacing to low-output pacing
- Select Normal sinus rhythm scenario and repeat steps 2-10
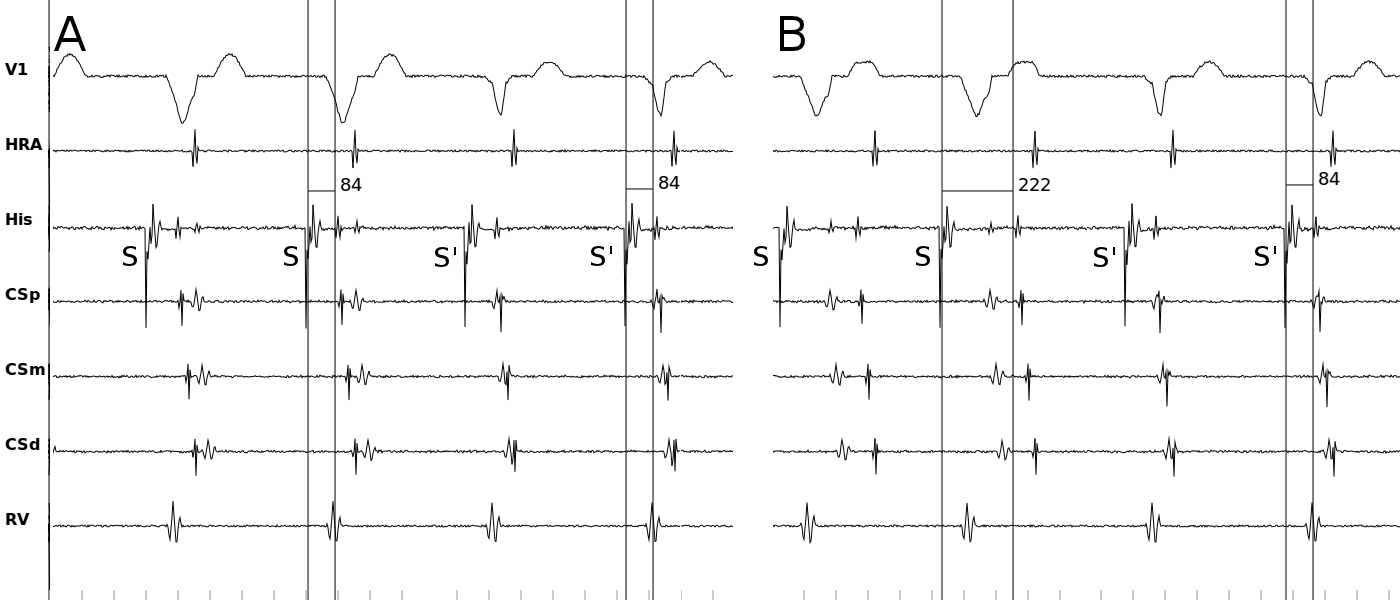
Simulated surface and intracardiac signals during para Hisian pacing. (A) Para Hisian pacing in the presence of a septal pathway (Septal pathway scenario). The VA interval is the same during low amplitude pacing (the first two beats, wide QRS complex) and high amplitude pacing (the last two beats, narrow complex), consistent with retrograde conduction over a septal pathway. (B) Para Hisian pacing in the AVNRT scenario. The VA interval is longer during low amplitude pacing (the first two beats, wide QRS complex) compared to the high amplitude pacing (the last two beats, narrow complex), consistent with retrograde conduction through the specialized conduction system.
Another pacing maneuver that can help differentiate a septal pathway from AV nodal conduction is pacing from RV apex and base. In the presence of an accessory pathway, VA timing is shorter during basilar pacing compared to apical pacing. The reverse is true for AV nodal conduction.
- Select Septal pathway scenario from the Advanced screen
- Select Pace location as "RV apex"
- Set S1 ← 600 ms
- Pace straight
- Pause and measure VA interval using the caliper
- Resume
- Stop pacing
- Select Pace location as "RV base"
- Repeat steps 3-7
- Compare VA timing during apical pacing to basal pacing
- Select Normal sinus rhythm scenario and repeat steps 2-10
The presence of a large excitable gap in concealed (retrograde-only) decremental septal pathways often results in the spontaneous induction of a narrow complex tachycardia called Permanent Reciprocating Junctional Tachycardia (PJRT), which is in fact a misnomer as the tachycardia is neither permanent nor junctional. As a consequence of the decremental properties of the accessory pathway in this model, ventricular overdrive pacing entrains the tachycardia with long PPI, ΔVA>85 ms and possibly a VAAV response.
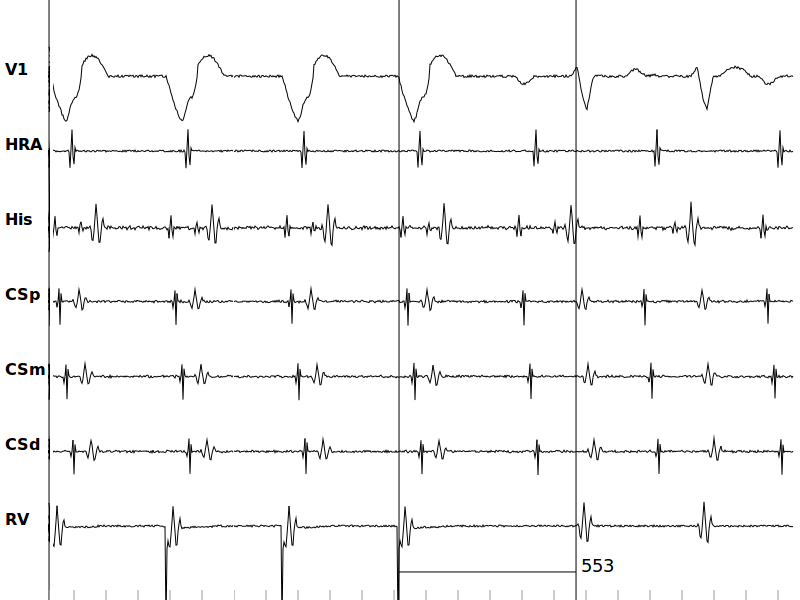
Simulated surface and intracardiac signals in the PJRT scenario. Ventricular overdrive pacing entrains the tachycardia with long PPI, ΔVA>85 ms and a VAAV response.
Wide Complex Tachycardias
Wide complex tachycardia (WCT) can also pose a difficult diagnostic challenge. Here, we look at two different WCT and their response to atrial pacing. We model atriofascicular pathways (Mahaim fibers) by adding a decremental unidirectional link between the atrium and RV apex. Atrial extrastimuli initiates an antedromic reciprocating tachycardia (ART) using the accessory pathway with a left bundle branch block (LBBB) morphology. A His refractory atrial premature beat that advances the next ventricular complex and resets the tachycardia proves that the accessory pathway participates in tachycardia.
- Select Atriofascicular pathway scenario from the Advanced screen
- Induce tachycardia
- Pause and measure AH interval (A in HRA to H) using the caliper
- Resume
- Set S1 ← AH and the number of beats in the S1 train ← 2
- Set the pace site at HRA
- Set the sense site at HRA
- Pace & Pause
- Measure HH to confirm His-refractoriness
- Measure VV interval
- Decrease S1 by 10 ms
- Repeat 8-11 until tachycardia terminates or VV changes
Another WCT with LBBB morphology is the Bundle Branch Reentrant (BBR) tachycardia, which is modeled by adjusting the refractoriness of the link between His and LV (i.e. the left bundle). The reentry circuit is composed of the right bundle, transseptal conduction, and retrograde conduction through the left bundle. Atrial overdrive pacing dissociates the atrial activity from the ventricles, which is highly suggestive of ventricular tachycardia.
Simulated surface and intracardiac signals during WCT. (A) His refractory atrial premature complex delivers during ART advances next ventricular activity and resets the tachycardia, consistent with the presence of an accessory pathway (Atriofascicular pathway scenario). (B) Bundle branch reentry with LBBB pattern (VT scenario). Atrial overdrive pacing dissociates atrial activity from the ventricular signal. Note that the His potential precedes the ventricular activity and is also dissociated from the atria.